Eye conditions
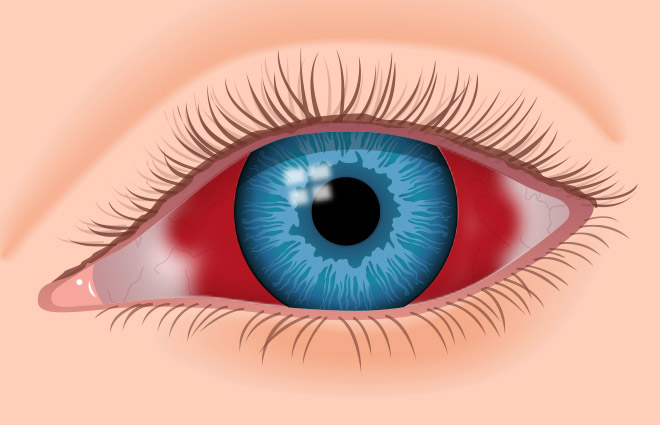
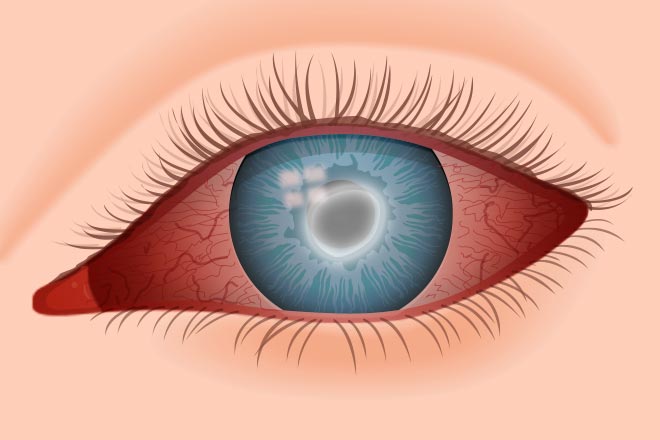
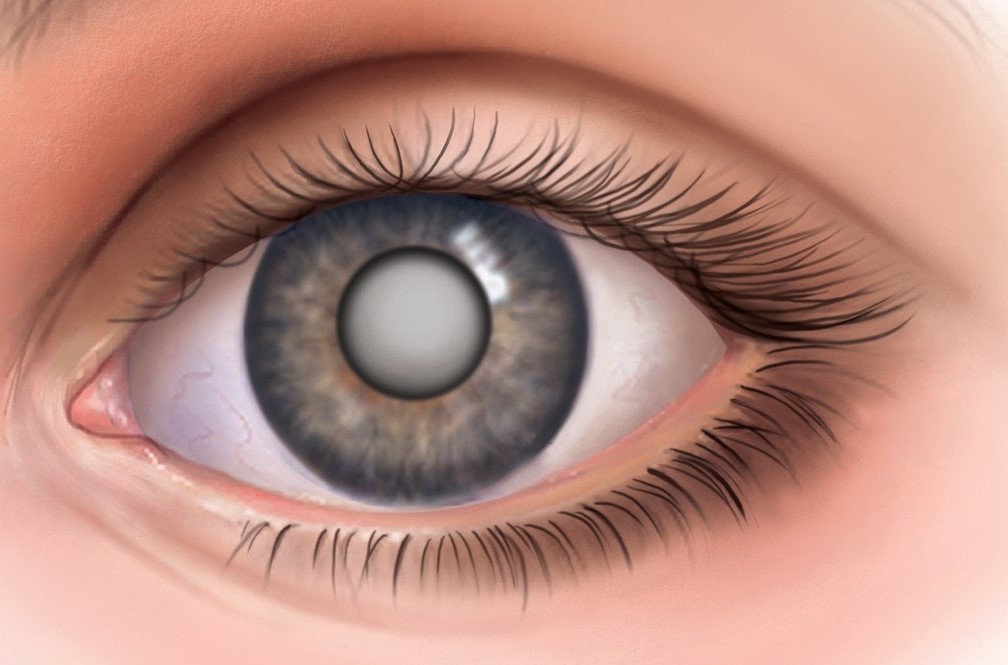
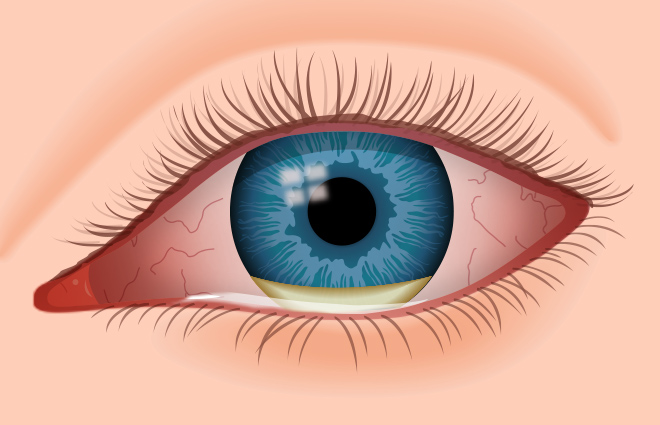
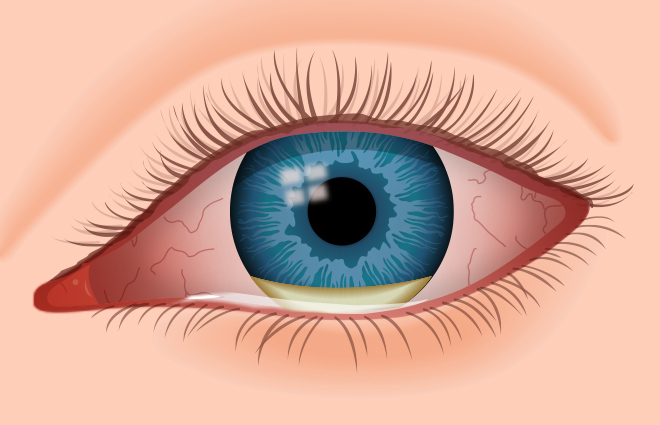
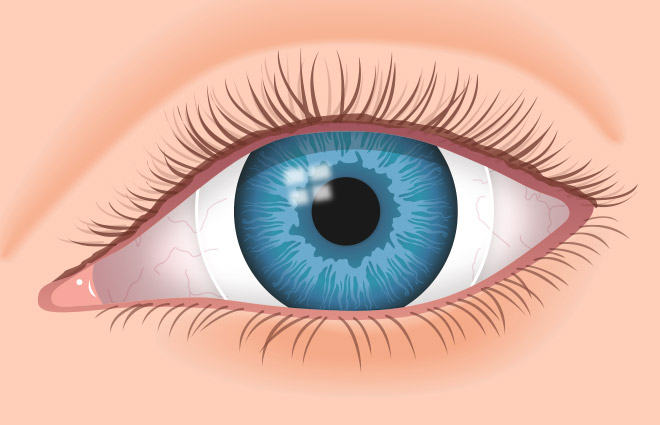
Red eye
Read more
Red eye is inflammation of the thin, clear covering of the white of the eye and the inside of the eyelids (conjunctiva). Anything that triggers inflammation will cause these conjunctival blood vessels to dilate. This is what causes red, bloodshot eyes. Red eye is frequently accompanied by eye pain, blurred vision, and sensivity to light. Often, eye pain that feels like something is in the eye actually is caused by irritation or inflammation of the front surface of the eye. Watery, burning, itchy eyes with sensitivity to light are the most common symptoms. There are many causes of red eye which must be investigated by an ophthalmologist.
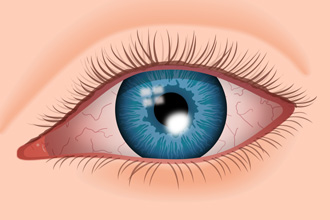
Conjuntivitis
Read more
Conjuntitivitis (pink eye) is inflammation of the thin, clear covering of the white of the eye and the inside of the eyelids (conjunctiva). The primary types of conjunctivitis, based on cause, are: viral (caused by a virus), bacterial (caused by bacteria) and allergic (caused by eye irritants such as pollen, dust and animal dander among susceptible individuals). One or both eyes can be affected. Red, burning, itchy eyes are the most common symptoms. In same cases there is a sticky, yellow or greenish-yellow eye discharge in the corner of the eye, this discharge can be severe enough to cause the eyelids to be stuck together when you wake up.
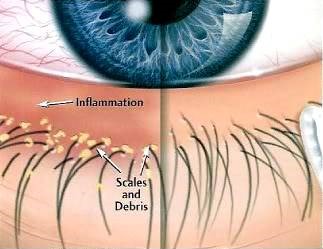
Blepharitis
Read more
Blepharitis is a common eye condition characterized by chronic inflammation of the eyelid, usually where eyelashes grow, resulting in inflamed, irritated, itchy, and reddened eyelids. It can be caused by the oil glands at the base of the eyelashes becoming clogged, a bacterial infection, allergies or other conditions. Blepharitis usually does not cause permanent eyesight damage. Long-term untreated blepharitis can lead to eyelid scarring, excess tearing, difficulty wearing contact lenses, development of a stye (an infection near the base of the eyelashes, resulting in a painful lump on the edge of the eyelid) orchronic pink eye.
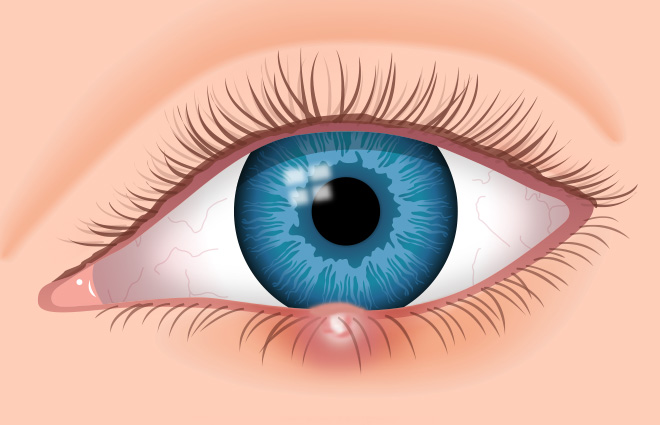
Stye – Chalazion
Read more
A stye develops when an oil gland at the edge of an eyelid becomes infected. Resembling a pimple on the eyelid, a stye can grow on the inside or outside of the lid. Stay is an infection near the base of the eyelashes, resulting in a painful lump on the edge of the eyelid. It is caused by long-term chronic eyelid inflammation.
Often mistaken for a stye, a chalazion is an enlarged, blocked oil gland in the eyelid. A chalazion mimics a stye for the first few days, then turns into a painless hard, round bump later on.
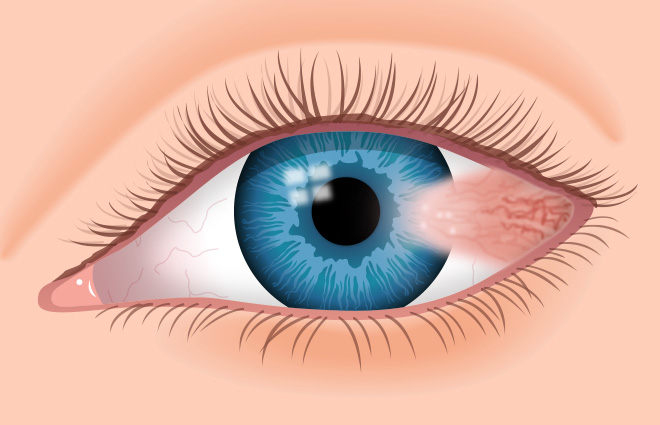
Pterygium
Lees verder
A pterygium is an elevated, wedged-shaped bump on the eyeball that starts on the white of the eye (sclera) and can invade the cornea. It´s benign (non-cancerous) growth, but it can permanently disfigure the eye. Large or growing pterygia often cause a gritty, itchy or burning sensation or the feeling something is “in” the eye (called a foreign body sensation). Although ultraviolet radiation from the sun appears to be the primary cause for the development and growth of pterygia, dust and wind are sometimes implicated too, as is dry eye disease. Pterygia usually occur on the side of the eye closer to the nose, but they can also develop on the side closer to the ear as well and can affect one eye or both eyes.
Keratitis – corneal ulcer
Read more
Keratitis is a condition in which the eye´s cornea, the front part of the eye, becomes inflamed. The condition is often marked by moderate to intense pain and usually involves any of the following symptoms: pain, impaired eyesight,sensivity to light, red eye and a ‘gritty’ sensation. Most cases of keratitis and corneal ulcer are due to a bacterial infection that invades the cornea — often following eye injury, trauma or other damage. Besides bacterial infection, other causes of corneal ulcers are fungi, herpes virus and parasites. If the ulceration is in the central cornea, the condition usually takes longer to go away, and vision may be reduced permanently due to scarring.
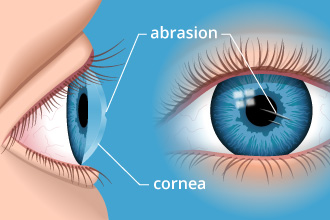
Corneal abrasion
Read more
A corneal abrasion (scratched cornea or scratched eye) is one of the most common eye injuries. A scratched cornea often causes significant discomfort, red eyes and hypersensivity to light. Corneal abrasions result from a disruption or loss of cells in the top layer of the cornea. The cornea is the clear front surface of the eye, and part of its job is to focus light, enabling you to see. A healthy cornea is essential for good vision. In addition to disrupting vision, a scratched cornea makes your eye more susceptible to infection. Many corneal abrasions aren’t caused by a noticeable traumatic event, such as getting poked in the eye. Sand, dust and other small particles can cause a corneal abrasion as well, especially if you rub your eyes.
Corneal dystrophy
Read more
Corneal dystrophies are a group of genetic, often progressive, eye disorders in which abnormal material often accumulates in the clear (transparent) outer layer of the eye (cornea). Corneal dystrophies may not cause symptoms (asymptomatic) in some individuals; in others they may cause significant vision impairment. The age of onset and specific symptoms vary among the different forms of corneal dystrophy. The disorders have some similar characteristics; most forms of corneal dystrophy affect both eyes (bilateral), progress slowly, do not affect other areas of the body, and tend to run in families.
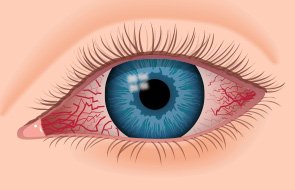
Epiescleritis and Scleritis
Read more
Episcleritis is a benign, self-limiting inflammatory disease affecting part of the eye called the episclera. The episclera is a thin layer of tissue that lies between the conjuntiva and the connective tissue layer that forms the white of the eye (sclera). Episcleritis is a common condition, and is characterized by the abrupt onset of mild eye pain and redness. Most cases of episcleritis have no identifiable cause, although a small fraction of cases are associated with various systemic diseases.
Scleritis is a serious, chronic, painful and potentially blinding inflammatory disease that affects the white outer coating of the eye, known as the sclera. The disease is often contracted through association with other systemic diseases of the body, usually an autoimmune disease. Scleral inflammation (scleritis) may occur in one or both eyes. Intense dull pain is a hallmark symptom.
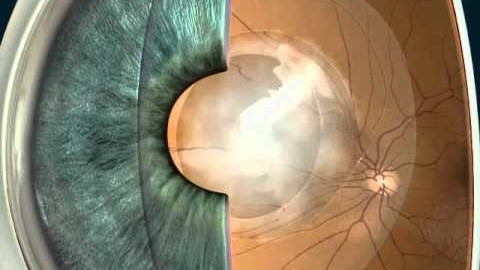
Cataract
Read more
A cataract is a clouding of the eye’s natural lens, which lies behind the iris and the pupil. A cataract starts out small and at first has little effect on your vision. You may notice that your vision is blurred a little, like looking through a cloudy piece of glass or viewing an impressionist painting. A cataract may make light from the sun or a lamp seem too bright or glaring. Or you may notice when you drive at night that the oncoming headlights cause more glare than before. Colors may not appear as bright as they once did. When symptoms begin to appear, you may be able to improve your vision for a while using new glasses,magnification, appropriate lighting or other visual aids.Think about surgery when your cataracts have progressed enough to seriously impair your vision and affect your daily life.
Secondary cataract
Read more
Sometimes, people who have their vision successfully restored with cataract surgery experience a second decline in their eyesight several weeks or months after their cataract procedure. The crystalline lens of the eye is enclosed in a clear membrane called the lens capsule. A significant portion of the lens capsule that’s in front of the lens is removed during cataract surgery to enable the surgeon to gain access to the cloudy lens (the cataract), break it up, remove it, and replace it with a clear intraocular lens. The posterior portion of the lens capsule (the part behind the lens) is left intact during cataract surgery, and the new lens is implanted directly in front of it. In a small percentage of people who have cataract surgery, the posterior lens capsule becomes cloudy several months or even years after surgery. The medical term for this is posterior capsular opacification, secondary cataract or after-cataract.
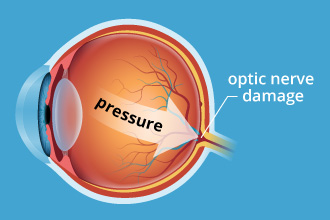
Glaucoma
Read more
Glaucoma refers to a group of related eye disorders that all cause damage to the optic nerve that carries information from the eye to the brain. Glaucoma usually has few or no initial symptoms. In most cases, glaucoma is associated with higher-than-normal pressure inside the eye — a condition called ocular hypertension. But it also can occur when intraocular pressure is normal. If untreated or uncontrolled, glaucoma first causes peripheral vision loss and eventually can lead to blindness. The two major categories of glaucoma are open-angle glaucoma and narrow angle glaucoma. The “angle” in both cases refers to the drainage angle inside the eye that controls the outflow of the watery fluid (aqueous) that is continually being produced inside the eye. If the aqueous can access the drainage angle, the glaucoma is known as open angle glaucoma. If the drainage angle is blocked and the aqueous cannot reach it, the glaucoma is known as narrow angle glaucoma. Glaucoma is the second-leading cause of blindness in the world (behind cataracts).
Uveitis
Read more
Uveitis is inflammation of the uvea — the middle layer of the eye that consists of the iris ciliary body and choroid. Uveitis can have many causes, including eye injury and inflammatory diseases. Exposure to toxic chemicals such as pesticides and acids used in manufacturing processes also can cause uveitis. Many cases of uveitis are chronic, and they can produce numerous possible complications, including clouding of the cornea, cataracts, elevated eye pressure, glaucoma, swelling of the retina or retinal detachment. These complications can result in permanent vision loss. About half of all uveitis cases don’t have an obvious cause. Symptoms of anterior uveitis include light sensitivity, decreased visual acuity, eye pain and red eyes.
.
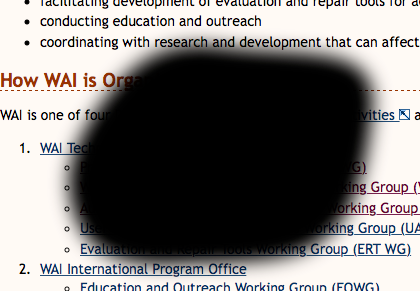
Eye floaters and black spots in vision
Read more
Eye floaters are those tiny spots, specks, flecks and “cobwebs” that drift aimlessly around in your field of vision. Floaters and spots typically appear when tiny pieces of the eye’s gel-like vitreous break loose within the inner back portion of the eye. When we are born and throughout our youth, the vitreous has a gel-like consistency. But as we age, the vitreous begins to dissolve and liquefy to create a watery center. Some undissolved gel particles occasionally will float around in the more liquid center of the vitreous. These particles can take on many shapes and sizes to become what we refer to as “eye floaters.” You’ll notice that these spots and eye floaters are particularly pronounced if you gaze at a clear or overcast sky or a computer screen with a white or light-colored background. You won’t actually be able to see tiny bits of debris floating loose within your eye. Instead, shadows from these floaters are cast on the retina as light passes through the eye, and those tiny shadows are what you see. Noticing a few floaters from time to time is not a cause for concern. However, if you see a shower of floaters and spots, especially if they are accompanied by flashes of light, you should seek medical attention immediately from an eye care professional.
Retinal detachment
Read more
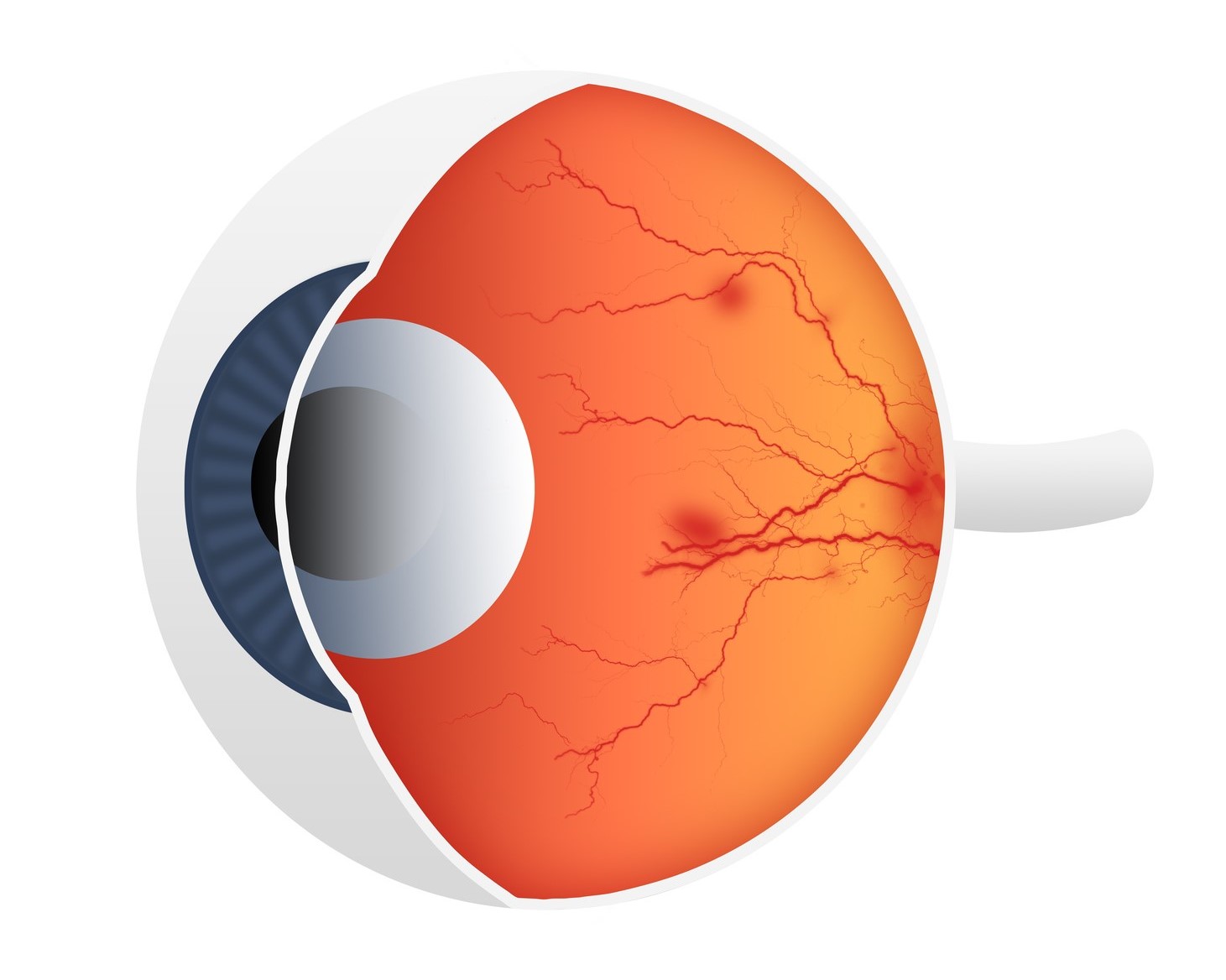
Retinal detachment occurs when the thin lining at the back of your eye called the retina begins to pull away from the blood vessels that supply it with oxygen and nutrients. The retina lies at the back of your eye and sends signals to the brain, allowing it to see. Without a blood supply, the nerve cells die which leads to a loss of sight. Most people will experience warning signs that indicate their retina is at risk of detaching before they lose their sight. These include: the sudden appearance of floaters – black dots, specks or streaks that float across your field of vision (usually only one eye is affected), sudden short flashes of light in the affected eye lasting no more than a second and blurring or distortion of your vision. Most people describe this as a shadow or “black curtain” spreading across their vision. Without prompt treatment, it will lead to blindness in the affected eye.
Diabetic eye disease ( diabetic retinopathy)
Read more
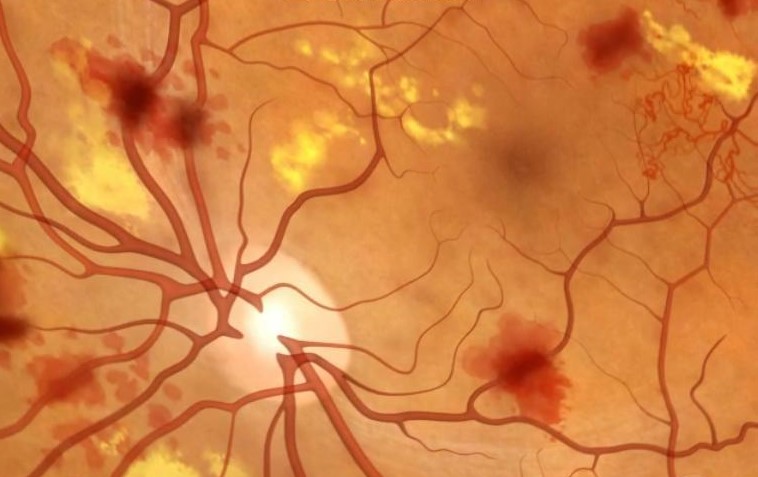
Uncontrolled diabetes allows unusually high levels of blood sugar (hyperglycemia) to accumulate in blood vessels, causing damage that hampers or alters blood flow to your body’s organs — including your eyes. Eye damage occurs when chronically high amounts of blood sugar begin to clog or damage blood vessels within the eye’s retina, which contains light-sensitive cells (photoreceptors) necessary for good vision. Once high blood sugar damages blood vessels in the retina, they can leak fluid or bleed. This causes the retina to swell and form deposits in early stages of diabetic retinopathy. In later stages, leakage from blood vessels into the eye’s clear, jelly-like vitreous can cause serious vision problems and eventually lead to blindness.
Hypertensive retinopathy
Read more
The retina is the tissue layer located in the back of your eye. This layer transforms light into nerve signals that are then sent to the brain for interpretation. When your blood pressure is too high, the retina’s blood vessel walls may thicken. This may cause your blood vessels to become narrow, which then restricts blood from reaching the retina. In some cases, the retina becomes swollen. Over time, high blood pressure can cause damage to the retina’s blood vessels, limit the retina’s function, and put pressure on the optic nerve, causing vision problems. This condition is called hypertensive retinopathy. Most patients with hypertensive retinopathy have no symptoms. However, some may report decreased or blurred vision and headaches.
Age Related Macular Degeneration (AMD)
Read more
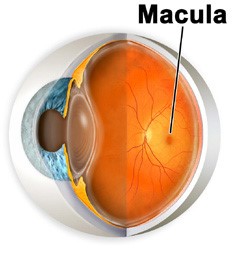
Age-related macular degeneration — also called macular degeneration, AMD or ARMD — is deterioration of the macula, which is the small central area of the retina of the eye that controls visual acuity. The health of the macula determines our ability to read, recognize faces, drive, watch television, use a computer, and perform any other visual task that requires us to see fine detail. Macular degeneration is diagnosed as either dry or wet. Gradual central vision loss typically occurs. With wet macular degeneration, new blood vessels grow beneath the retina and leak blood and fluid. This leakage causes permanent damage to light-sensitive retinal cells, which die off and create blind spots in central vision.
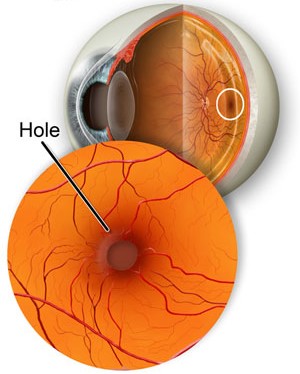
Macular hole
Read more
The macula is a very small spot in the center of the back of the eye (retina). Light focuses to a sharp point at the macula, which is the only area of the eye that sees crystal clear. When a macular hole develops, most people notice a sudden decrease in vision in one eye, the vision becomes blurry and distorted. Because macular holes often are related to aging processes, they are more likely to develop if you are over age 60. A macular hole sometimes can resolve without intervention, but most should be treated to prevent permanent vision loss.
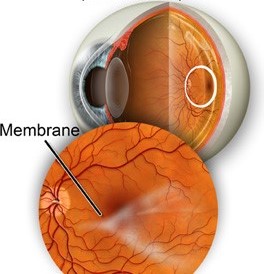
Macular pucker – Epiretinal membrane
Read more
A macular pucker is a layer of scar tissue that grows on the surface of the retina, particularly the macula, which is the part of your eye responsible for detailed, central vision. The macula is the small area at the center of the eye’s retina that allows you to see fine details clearly. As light rays enter your eye, the retina converts the rays into signals, which are sent through the optic nerve to your brain where they are recognized as images. The macula normally lies flat against the back of the eye. When wrinkles, creases or swelling affect the macula, vision can become blurry and distorted and you may even have a blind spot in your central vision.
.
Macula oedema
Read more
Macular edema is swelling or thickening of the eye’s macula, the part of your eye responsible for detailed, central vision. The macula is a very small area at the center of the retina—a thin layer of light-sensitive tissue that lines the back of the eye. The macula is responsible for your pinpoint vision, allowing you to read, sew or recognize a face. Macular edema develops when blood vessels in the retina are leaking fluids. The macula does not function properly when it is swollen. Vision loss may be mild to severe, but in many cases, your peripheral (side) vision remains. Macular edema is often a complication of diabetic retinopathy, and is the most common form of vision loss for people with diabetes—particularly if it is left untreated.
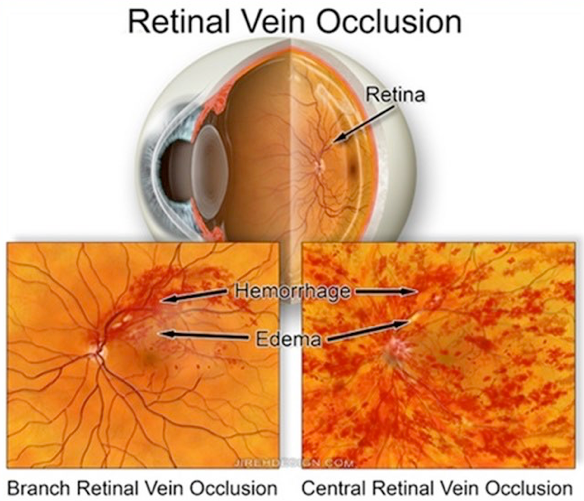
Retinal vascular occlusion
Read more
Retinal vascular occlusion affects the retina, the light- sensitive layer of tissue that lines the back of your eye. The retina is vital for vision. The vascular system includes blood vessels called arteries and veins, which transports blood throughout your body, including your eyes. Your retina requires a constant supply of blood to make sure your cells get enough nutrients and oxygen. Blood also removes the waste your retina produces. However, it’s possible for one of the vessels carrying blood to or from the retina to become blocked or have a blood clot. This is called an occlusion. The occlusion can cause blood or other fluids to build up and prevent the retina from properly filtering light. When light is blocked or fluids are present, a sudden loss of vision can occur. The severity of vision loss may depend on where the blockage or clot occurred.
.
Ocular migraine
Read more
Ocular migraines are painless, temporary visual disturbances that can affect one or both eyes. Though they can be frightening, ocular migraines are typically harmless and self-resolve without medication within 20 to 30 minutes.If an ocular migraine-like vision disturbance is followed by a throbbing, usually one-sided headache, this is called a “migraine with aura” (classic migraine). You might see a small, enlarging blind spot (scotoma) in your central vision with bright, flashing or flickering lights (scintillations), or wavy or zig-zag lines surrounding the blind spot. The blind spot usually enlarges and may move across your field of vision. This entire migraine phenomenon may end in only a few minutes, but usually lasts up to 30 minutes.
Double vision – diplopia
Read more
The ability to see a single image with two eyes involves a complex system of muscles, nerves and other eye parts. When two eyes correctly and accurately point and focus at the same time, we see only one image of the world. When two eyes point and focus differently from each other, double vision may happen.
Temporary episodes of double vision can happen for many reasons, including drinking too much alcohol or being overly tired. This type of short-term double vision is usually not cause for worry. But if the diplopia is long-lasting or keeps coming back, reasons for it can include: stroke, cranial nerve palsies, head injury, brain tumor, brain swelling or brain aneurysm, corneal irregularities,dry eyes, refractive surgery, cataracts.
Drye eye
Read more
Dry eye syndrome is a chronic and typically progressive condition. Dry eye is caused by a chronic lack of sufficient lubrication and moisture on the surface of the eye. Consequences of dry eyes range from subtle but constant eye irritation to significant inflammation and even scarring of the front surface of the eye.
Symptoms of dry eye syndrome include: burning, aching sensation, itchy, heavy, fatigued or sore eyes, red eyes, light sensitivity and blurred vision. Another common symptom is something called a foreign body sensation — the feeling that grit or some other object or material is “in” your eye. In addition to these symptoms, dry eyes can cause inflammation and (sometimes permanent) damage to the surface of the eye.
Eyelids pathology and tumors
Read more
There are several different types of eyelid growths. Nevus and papilloma are the most common. Benign and malignant tumors can form on the eyelids.
Accurate diagnosis by an ophthalmologist is based on history and clinical examination. When in doubt, any suspicious lesion should undergo biopsy.
The majority of eyelid papillomas can be observed unless they rapidly grow, cause mechanical disruption of eyelid function or are cosmetically disfiguring, in which case they can be completely excised.
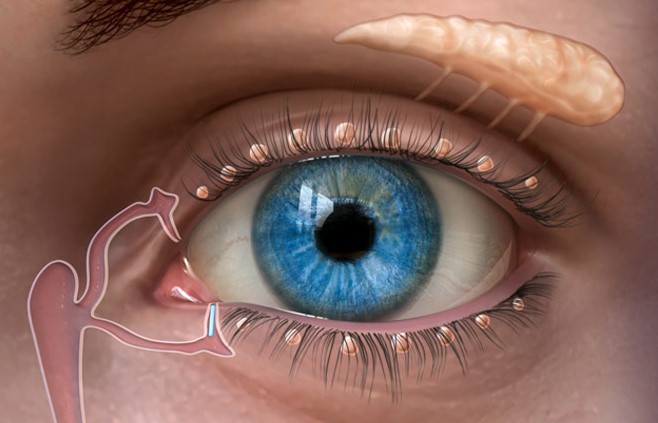
Epiphora – lachrymation
Read more
Watering eyes occur if too many tears are produced or if they cannot drain away properly. The problem can affect anyone, but it’s most common in young babies and people older than 60. It can cause blurred vision, sore eyelids and sticky eyes. The problems that can cause extra tears to be produced include: inflammation of the edges of the eyelids (blepharitis), the lower eyelid sagging away from the eye (ectropion) – this makes it difficult for tears to reach the drainage ducts, eyelids that roll inwards (entropion), blocked or narrowed tear ducts, eye irritation (for example, from chemical fumes or grit), an eye infection or allergy.
Contact lens complications
Read more
There are many complications that the contact lens wearer may experience; complications that are either directly induced or complications that represent existing problems aggravated by the contact lens wear. The mechanisms by which the contact lenses induce alterations are: trauma, decreased corneal oxygenation, reduced corneal and conjunctival wetting, stimulation of allergic and inflammatory responses, and infection.